Autoclave principle, working and its types
Autoclave principle, working and its types
Steam Sterilizer / Autoclave :
The autoclave is a sealed device (similar to a pressure cooker) that kills microorganisms using saturated steam under pressure .
Principle :
The use of moist heat facilitates the killing of all microorganisms, including heat-resistant endospores which is achieved by heating the materials inside the device at temperatures above the boiling point of water.
Method :
Moist heat in the form of steam under pressure causes the denaturation & coagulation of proteins by following steps .
1.Conditioning : The usual procedure is to heat at 1.1 kilograms/square centimeter (kg/cm2) [15 pounds/square inch (lb/in.)] steam pressure, which yields a temperature of 121°C. At 121°C, the time of autoclaving to achieve sterilization is generally considered to be 15-20 min, depending on the volume of the load.
2. Exposure : Direct saturated steam contact is the basis of the steam sterilization process. For a specified time and at a required temperature, the steam must penetrate every fiber and reach every surface of the items to be sterilized.
3. Condensation : When steam enters the sterilizer chamber under pressure, it condenses on contact with cold items. This condensation liberates heat, simultaneously heating and wetting all items in the load and thereby providing the two requisites : moisture & heat .
4. Drying: At the end of the cycle, re-evaporation of water condensate must effectively dry contents of the load to maintain sterility; the water is dried from the sterilized pack or item.
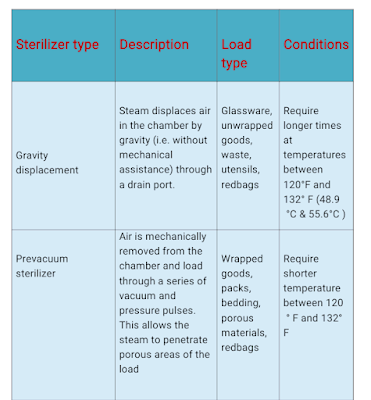
Types of Autoclave :
1. Gravity displacement sterilizer :
Principle :
A steam sterilizer that uses steam in a downward motion to remove air from the sterilizing chamber. Air exits near front lower drain.
Method :
It contains two shells that form a jacket and a chamber. Steam fills the jacket that surrounds the chamber. After the door is tightly closed, steam enters the chamber at the back, near the top, and is deflected upward. Air is more than twice as heavy as steam. Thus by gravity, air goes to the bottom and steam floats on top.The air passes through a filtering screen to a waste line.
Many gravity displacement steam sterilizers operate on a standard cycle of 250° F to 254° F (121° C-123° C) at a pressure of 15 to 18 pounds per square inch (psi). The size and contents of the chamber determine the exposure period; the minimum exposure time is 15 minutes.
2. Pre-vacuum sterilizer :
Principle : A faster steam sterilizer that removes air by a vacuum before filling the chamber with steam. Also known as dynamic air removal steam sterilization.
Method : In this high-vacuum sterilizer, air is almost completely evacuated from the chamber before the sterilizing steam is admitted using a pump and a steam injector system. A vacuum period of 8 to 10 minutes effectively removes the air to minimize the steam penetration time. As a result, the sterilizing steam almost instantly penetrates the center of the packages when admitted to the chamber.
A post-vacuum cycle draws moisture from the load to shorten the drying time. The Bowie-Dick test is performed daily to ensure that the air vacuum pump is functioning properly.
Temperatures in the pre-vacuum sterilizer are controlled at 270° F to 276° F (132° C-135.5° C) at a pressure of 27 psi. All items are exposed to a temperature of at least 270° F (132° C) for a minimum of 4 minutes. A complete cycle takes approximately 15 to 30 minutes, depending on the sterilizer's capacity.
FLASH (IMMEDIATE-USE) STERILIZER
A high-speed pre-vacuum sterilizer is used in the operating room and in other areas of the hospital to sterilize items for immediate use. Steam sterilization using an abbreviated cycle at a high temperature is necessary for rapid sterilization.
However, advanced technology leading to new materials and complex equipment has led to equally complex guidelines for ensuring patient safety.
In the past, the term flash sterilization was used to describe the process of a shortened sterilization cycle for uncovered items. Now, however, there are situations in which items are covered in a variety of ways, even for immediate use following sterilization.
A standards committee composed of members of accredit-action bodies, research professionals, and key health professionals agreed in 2010 that the term flash sterilization does not reflect the complexity of sterilization for immediate use. The term has been replaced with immediate-use sterilization.
Standards for immediate-use sterilization have been adapted by the Association of Surgical Technologists as well as other
professional organizations.
The statement on adaptation to the new terminology can be found on the AAMI website, http://www.aami.org/
publications/standards/ST79_Immediate_Use_Statement.pdf.
This website also provides references for the standards and practices currently approved by accrediting and professional agencies.
Sterilizers employed for immediate use are usually located just outside the operating suite, in the sub sterile or core area.
This type of sterilizer is used only when no alternative is available. Items are sterilized just before use. Ideally, items to be sterilized for immediate use should be in a covered metal tray.
However, some immediate-use sterilizers can be used with a drying cycle that is suitable for items wrapped in a single layer of woven material. Unwrapped items coming from the an immediate-use sterilizer will be wet, as there is no drying cycle for unwrapped goods.