Pros and cons of washer sterilizer over manual cleaning with refrences
Manual Cleaning:
Manual cleaning involves physically removing dirt, debris, and contaminants from surfaces using hands and basic cleaning tools, rather than relying solely on machines or automated systems.
Steps for Effective Manual Cleaning:
1. Gather Supplies: Collect all necessary cleaning supplies, including:
- Cleaning agents (detergents, disinfectants).
- Cleaning tools (mops, cloths, brushes, sponges).
- Personal protective equipment (gloves, masks).
- Clear the Area: Remove any items from surfaces that need cleaning.
- Pre-Cleaning Assessment: Inspect surfaces for visible dirt and specific cleaning needs.
- Dusting: Start by dusting surfaces to remove loose dirt and particles.
- Washing: Apply a cleaning solution to surfaces. Use appropriate techniques based on the surface type:
- For hard surfaces: Use a cloth or sponge to scrub and wipe.
- For delicate surfaces: Use softer materials to avoid damage.
- Rinsing: If required, rinse surfaces with clean water to remove cleaning agents.
- Drying: Allow surfaces to air dry or use a clean, dry cloth.
- After manual cleaning, apply a suitable disinfectant to surfaces to kill any remaining pathogens.
- Follow the manufacturer's instructions for contact time and safety precautions.
- Inspect: Check the area to ensure thorough cleaning has been achieved.
- Dispose of Waste: Properly dispose of any cleaning materials and waste.
- Wash Hands: Perform hand hygiene after cleaning to prevent cross-contamination.
Pros:
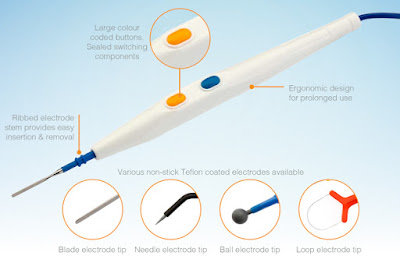
- Parts can be cleaned without complete immersion in solution
- Microsurgical & opthalmic instruments are cleaned through this method ; not put in washer sterilizer
- Additional cleaning equipment such as wash & rinse tank is not necessary
Cons:
- Cleaning efficacy is less
- Required additional time to complete
- Labor intensive process
- Cleaning solution consumption is higher
- Limitation on use of aggressive chemical
- Personnel requires PPE to prevent accidental spray from contaminated body fluids
- Cost analysis : 50 -60 thousands to buy ; 30,000 for staff monthly ; 30,000 for its maintainance & repair .
Washer sterilization:
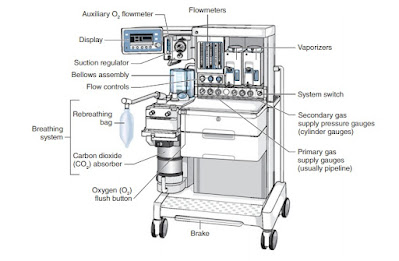
Washer sterilization refers to the use of specialized washing machines, often referred to as "washer-disinfectors" or "sterilizers," that clean and disinfect items using high temperatures and/or chemical agents. These machines are designed to handle instruments, surgical textiles, and other equipment that require strict sterilization protocols.
Types of Washer Sterilization
1. Thermal Disinfection:
- Mechanism: Uses high temperatures (usually above 80°C or 176°F) to kill microorganisms.
- Process: Items are washed with detergent, rinsed, and then subjected to a thermal disinfection cycle, which typically includes a final rinse with hot water.
- Applications: Commonly used for heat-resistant instruments and textiles.
- Mechanism: Utilizes chemical agents (e.g., hydrogen peroxide, peracetic acid) in the wash cycle to achieve disinfection.
- Process: Items are cleaned and then submerged in or exposed to the chemical solution, often in a closed system that enhances contact time.
- Applications: Suitable for heat-sensitive items that cannot withstand high temperatures.
- Mechanism: Combine washing, disinfecting, and sterilizing functions into a single machine.
- Process: Items undergo cleaning, rinsing, and sterilization, often using steam or other sterilizing agents.
- Applications: Ideal for surgical instruments and devices that require full sterilization.
Steps for Washer Sterilization
Pre-Cleaning:
- Immediate Rinse: Rinse instruments and textiles immediately after use to remove blood and debris.
- Soaking: If immediate washing isn't possible, soak items in a solution to prevent drying of contaminants.
Loading:
- Proper Arrangement: Load items in a way that allows for optimal water and detergent circulation. Avoid overcrowding to ensure effective cleaning.
Selection of Cycle:
- Choose the Right Cycle: Select the appropriate cycle based on the items being processed (e.g., standard wash, thermal disinfection, or sterilization).
Monitoring:
- Temperature and Time: Regularly monitor the temperature and cycle times to ensure they meet established protocols.
- Biological Indicators: Use biological indicators (e.g., spore tests) to verify the effectiveness of the sterilization process.
Post-Cleaning Handling:
- Inspect for Residue: Check items for any remaining residues or contaminants after the cycle.
- Proper Storage: Store sterilized items in a clean, dry, and sterile environment to maintain their sterility.
Maintenance of Equipment:
- Regular Maintenance: Conduct routine maintenance on washer sterilizers to ensure proper functioning and prevent breakdowns.
- Calibration and Validation: Regularly calibrate equipment and validate processes to maintain compliance with sterilization standards.
Pros:
- It can handle a large capacity of instruments
- It has a fully automated cycle
- It result in reduced instrument handling.
- It can include thermal disinfection from 176 to 194 degrees Fahrenheit (80 to 90 degrees Celsius)
- Instruments may be safely handle without gloves
Cons :
- It depends on liquid spray as the method for removing dirt and debris.
- If parts of instruments are not exposed directly to the spray, they may not get cleaned.
- More costly to purchase
- Cost - 40 - 50 lakh to buy with automatic repair option
The first, and perhaps most significant, is the advancement made in upgrading from manual or decontamination to an automatic washer/disinfector alone can help CPD develop a quality decontamination system that will do more for less.
The second advancement has been in automating material handling systems that support automated single-chamber washers, and containing or reducing the amount of staff required to keep them humming.
References :
1 . Efficacy of a Washer-Disinfector in Eliminating Healthcare-Associated Pathogens from Surgical Instruments , William A. Rutala ,Maria F. Gergen & David J. Weber by cambridge university , 10 may 2016
2. Evaluation of the effectiveness of an enzymatic cleaner & glutaraldehyde-based disinfectant for chemothermal processing of flexible endoscopes in washer-disinfectors in …B Zühlsdorf, G KampItf Endoscopy 38 (06), 586-591, 2006
3. Natural bioburden levels detected on flexible gastrointestinal endoscopes after clinical use and manual cleaning Nancy S.ChuMSPatricia A.Antonoplos
4. Automating CPD Instrument Cleaning & Decontamination By Michael Cain